van Lent PLEM, Holthuysen AEM, van den Bersselaar LAM, van Rooijen N, Joosten LAB, van de Loo FAJ, van de Putte LBA, van den Berg WB. Phagocytic lining cells determine local expression of inflammation in type II collagen–induced arthritis.Arthritis & Rheumatism. 1996 Sep;39(9):1545–55.
Abstract
Objective . To investigate the in vivo role of phagocytic synovial lining cells in the local expression of inflammation in type II collagen–induced arthritis (CIA) in DBA/1J mice.
Methods . On various days before arthritis induction (day 7, 5, or 2), phagocytic lining cells were selectively depleted from the synovial layer by injecting multilamellar liposomes containing clodronate (dichloromethylene diphosphonate) directly into the knee joints. As controls, either PBS or PBS-laden liposomes were injected. CIA was induced by immunizing mice with heterologous bovine type II collagen in Freund’s complete adjuvant. Arthritis onset was synchronized by a single intraperitoneal injection of lipopolysaccharide; arthritis was evaluated in hematoxylin and eosin–stained knee joint sections. Chemotactic activity in synovial washout samples was detected in a Transwell chemotactic assay. Interleukin-1 (IL-1) and tumor necrosis factor α (TNFα) protein levels were measured in NOB-1 and L929 bioassays, respectively. IL-1 messenger RNA (mRNA) in synovial specimens was measured by reverse transcriptase–polymerase chain reaction. IL-1 was also detected immunohistologically in knee joint sections.
Results . In clodronate-laden liposome–treated, lining-depleted knee joints, there was significantly decreased inflammation compared with controls. Cell influx into the synovium was markedly decreased. Expression of IL-1 mRNA in the synovium was significantly reduced. IL-1 was detected only in some cells in the deeper synovial layer, in contrast to controls, in which large numbers of cells in the deeper synovial layer were stained. In synovial washouts from lining-depleted knee joints, biologically active IL-1 levels were reduced by 40% at 6 hours after arthritis induction. Most strikingly, chemotactic activity was highly decreased in these synovial washout samples. When IL-1 or TNFα was injected into the knee joints of immunized mice in which arthritis was not yet expressed, arthritis was not induced in the lining-depleted joints, whereas marked cell influx was found in control joints.
Conclusion . Our data indicate that phagocytic lining cells play a crucial role in the local expression of inflammation in systemically induced CIA. Phagocytic lining cells probably form an important source of chemotactic factors which are set free upon activation by IL-1 or TNFα.
| Clodronate Concentration | Total Lipid Concentration | Lipid Composition | Lipid Mole % | Liposome Type | Control Liposomes | Control Free Clodronate |
|---|---|---|---|---|---|---|
| 5 mg/ml | 23.5 mg/ml | EPC/chol | 84/16 | MLV | PBS | ND |
| Animal Description | Clodronate Dose | Dosing Method/Site | Target Phagocytes | Systemic Dosing? | Systemic Results |
|---|---|---|---|---|---|
| DBA/1 lac J, male, 10-12 w | 30 µg/6 µl | intra-articular/knee | eosin/hematoxylin stained MΦ | no | N/A |
Notes
- Liposome prep method cited— van Rooijen N, Sanders A. Liposome mediated depletion of macrophages: mechanism of action, preparation of liposomes and applications. Journal of Immunological Methods. 1994 Sep 14;174(1–2):83–93.
- Mice were given intra-articular injections of clodronate liposomes in one knee while either PBS or PBS liposomes were injected into the contralateral knee.
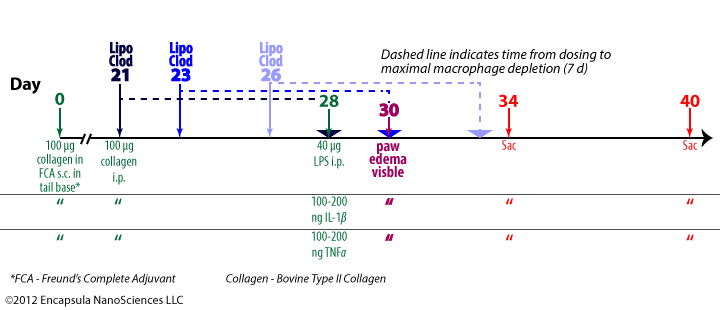
Experimental treatment protocol described in van Lent, et. al. , 1996. Macroscopic paw edema was visible by 2 days post-onset of arthritis (day 28). In separate experiments either IL-1β or TNFα instead of LPS was used to initiate arthritis on day 28.
- Hind paws became visibly swollen 2 days post-onset of arthritis at day 28.
- Mice were sacrificed either 6 days or 12 days post-onset of arthritis at day 28.
Results
- The total number of cells found in synovial fluid (exudate) did not decrease significantly from control values in arthritic animals that were treated with intra-articular liposomal clodronate either 7, 5 or 2 d prior to the onset of arthritis. The animals were sacrificed 6 d post-onset and the cell count (eosin/hematoxylin stained) was determined microscopically.
- The total number of cells found in synovial layer (infiltrate) in liposomal-clodronate-treated animals was only about 20-30% of the total cells found in control (PBS or PBS liposomes) animals.
- The synovial layer of liposomal clodronate treated animals showed about 75% reduction in both neutrophils and macrophages, although the ratio of macrophages to neutrophils did not change.
- The effect was observed only in the treated knee and not the contralateral knee of an animal and no differences were seen between animals that were treated at differing times before onset.
- Clodronate liposome treatment had no effect on hindpaw swelling of the treated limb.
- Similar responses were seen in animals that were sacrificed 12 days post-onset of arthritis.
- Synovial washouts of treated animals (7 d prior to onset) either 6 h or 48 h post-onset of arthritis showed a 70% (6 h) and 95% (48 h) reduction in their ability to stimulate migration of PMN.
- At 6 h post-onset, IL-1 β mRNA levels were reduced 4X in animals treated 7 d post-onset with clodronate liposomes compared to controls.
- At 6 h post-onset, IL-1 β protein level was reduced by about 40% in liposome treated animals compared to controls. At 2 d post-onset, IL-1 β was minimal in all groups.
- Clodronate liposome treatment completely abolished cell-influx (counted 2 d post-onset) into joints treated with either 100 or 200 ng IL-1 β or 100 or 200 ng TNF α injected on day 28 (instead of LPS).
- The authors suggested that they thought that clodronate-liposome mediated depletion of macrophages may enhance the arthritic response due to cytokine release as a result of macrophage death. Since this was not the case, they speculate that either cytokine release is minimal during depletion or the cytokines may have been contained in apoptotic bodies.
- The authors conclude that the cells of the synovial lining are the key sources of cytokine-induced influx of inflammatory cells post-onset of collagen-induced arthritis.